A fresh look at exercise intensity in pregnancy (without the stress of a heart rate tracker)
If you’ve ever Googled “should I monitor my heart rate while exercising during pregnancy?” you’re not alone. It’s one of the most common questions I get – and unfortunately, there’s a lot of outdated advice still floating around.
Let’s be clear: that whole “keep it under 140 bpm” rule? It belongs with scrunchies, perms and lacey maternity dresses. Cute in the 90s, but not helpful now.
As a fertility coach and women’s health professional, I’m here to break down what’s changed in the guidelines, why heart rate isn’t a reliable tool for every pregnant woman, and how to actually track your exercise intensity safely.
Where did the 140 bpm rule even come from?
Back in the 1990s, the American College of Obstetricians and Gynecologists (ACOG) recommended that pregnant women keep their heart rate under 140 beats per minute while exercising. That was based on what little research they had at the time.
But as more data emerged, it became clear that this one-size-fits-all number wasn’t cutting it. Every woman has a different level of fitness, a different pregnancy experience, and a unique heart rate response to exercise.
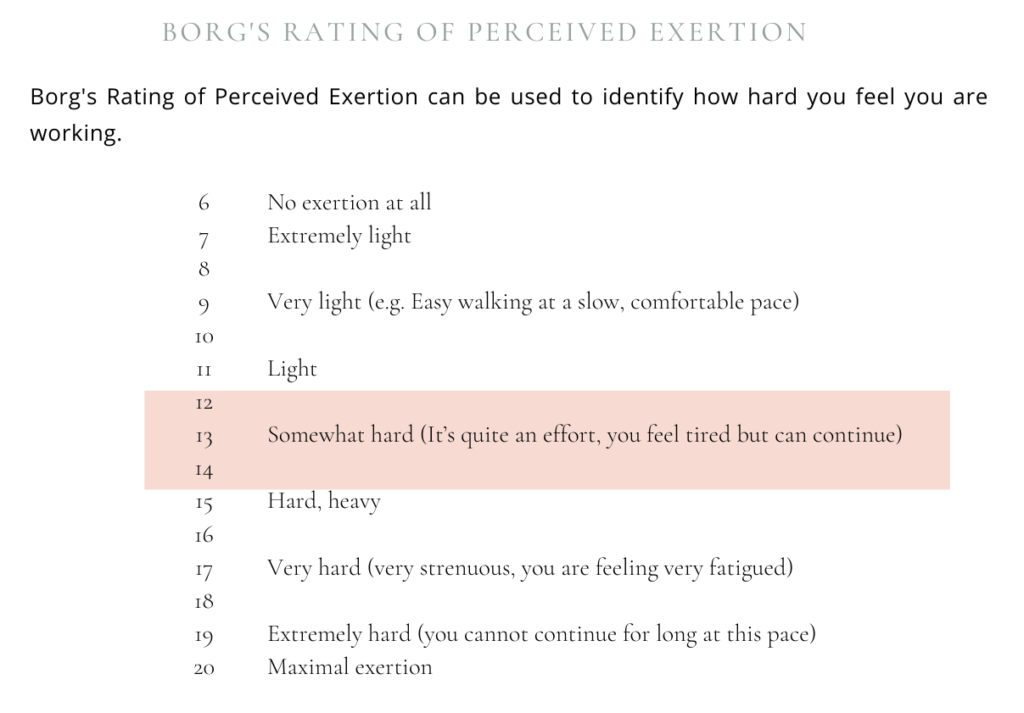
So, in 2002, ACOG officially ditched the 140 bpm rule in favour of something called the Borg Rating of Perceived Exertion. It’s a scale that helps you measure how hard you’re working based on how you feel, not what your smartwatch says.
How pregnancy changes your circulatory system
Before we dive into the Borg Scale, let’s talk about what happens to your body – especially your heart – during pregnancy.
Your blood volume increases by about 40% (that’s an extra 1.5 litres!) to support your growing baby. But while there’s more blood circulating, your red blood cells don’t increase at the same rate, which often leads to fatigue and low iron levels.
Your heart rate also naturally rises, especially early in pregnancy, which means you don’t have to do as much to get your heart pumping during a workout. This is why using heart rate alone to measure effort is completely unreliable in pregnancy.
So, what should you use instead?
Enter: the Borg Scale. Instead of focusing on your heart rate, you tune into how you feel. The goal? Aim for a “somewhat hard” effort; usually around 12–14 on the scale.
That might sound vague, but it’s actually super intuitive.
Here’s how to use it:
- If you can still hold a conversation while working out, you’re in a good zone.
- If you’re gasping for breath, red in the face and can’t talk, you’re pushing too hard.
- If you’re sweating and your body feels like it’s working but not overwhelmed, that’s the sweet spot.
This approach gives you permission to exercise in a way that works for you, and adjust as your pregnancy progresses.
Can you still work out during pregnancy?
Absolutely! – and in fact, regular movement is encouraged. Unless your doctor has advised otherwise, current ACOG guidelines recommend:
- 20–30 minutes of moderate-intensity exercise
- On at least 5 days a week
- Sessions under 45 minutes to avoid overheating or low blood sugar
You can mix cardio, stretching and strength training – or break it up into smaller chunks if that’s more realistic. The key is consistency, not perfection.
Already active pre-pregnancy? You can likely keep doing what you were doing, just dial it back as needed. New to exercise? Walking is a great way to start.
What if I’m an athlete or very active?
If you’re used to training hard, you might find the slower pace of pregnancy frustrating. But trust me, now is not the time to chase PBs.
While the Borg Scale still applies to you, it can help to work with a coach or healthcare provider to find the right balance between challenge and safety. In some cases, a heart rate monitor can be useful as one piece of the puzzle, but it shouldn’t be the only thing you rely on.
And remember: even the fittest woman can’t out-train the effects of pregnancy hormones on ligaments, joints and energy levels. Adaptability is your best friend.
Signs to stop exercising immediately
Exercise is generally safe during pregnancy, but there are red flags to watch for. Stop and consult your doctor if you experience:
- Vaginal bleeding or fluid loss
- Painful contractions
- Chest pain or shortness of breath
- Dizziness, headaches or fainting
- Calf pain or swelling
- Muscle weakness, balance issues or difficulty walking
- Sudden reduction in baby movements
- Severe fatigue or heart palpitations
These could indicate something more serious – and it’s always better to err on the side of caution.
Final thoughts: Listen to your body
Pregnancy is not the time for competition – not with others, and not with your past self.
Whether you’re hoping to conceive naturally again in future, or you’re just trying to stay healthy throughout pregnancy, the most important thing is to move in a way that supports your body and baby – without pushing beyond your limits.
So ditch the outdated rules. Trust your instincts. And work with professionals who understand natural fertility, safe pregnancy movement, and real-world exercise strategies.
If you’re ever unsure, that’s what your fertility coach and medical team are there for.

+ show Comments
- Hide Comments
add a comment